- Retrait gratuit dans votre magasin Club
- 7.000.000 titres dans notre catalogue
- Payer en toute sécurité
- Toujours un magasin près de chez vous
- Retrait gratuit dans votre magasin Club
- 7.000.000 titres dans notre catalogue
- Payer en toute sécurité
- Toujours un magasin près de chez vous
Description
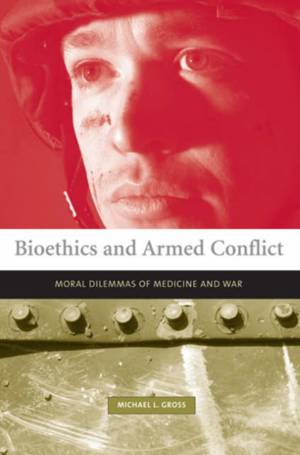
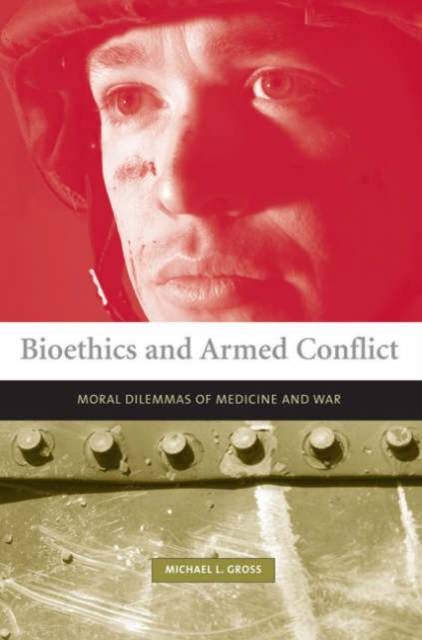
Is medical ethics in times of armed conflict identical to medical ethics in times of peace, as the World Medical Association declares? In Bioethics and Armed Conflict, the first comprehensive study of medical ethics in conventional, unconventional, and low-intensity war, Michael Gross examines the dilemmas that arise when bioethical principles clash with military necessity--when physicians try to save lives during an endeavor dedicated to taking them--and describes both the conflicts and congruencies of military and medical ethics.
Gross describes how the principles of contemporary just war, unlike those of medical ethics, often go beyond the welfare of the individual to consider the collective interests of combatants and noncombatants and the general interests of the state. Military necessity plays havoc with such patients' rights as the right to life, the right to medical care, informed consent, confidentiality, and the right to die. The principles of triage in battle conditions dictate not need-based treatment but the distribution of resources that will return the greatest number of soldiers to active duty. And unconventional warfare, including current wars on terrorism, challenges the traditional concept of medical neutrality as physicians who have sworn to do no harm are called upon to lend their expertise to interrogational torture or to the development of biological or chemical weapons. Difficult dilemmas inevitably arise during armed conflict, and medicine, Gross concludes, is not above the fray. Medical ethics in time of war cannot be identical to medical ethics in peacetime.
Spécifications
Parties prenantes
- Auteur(s) :
- Editeur:
Contenu
- Nombre de pages :
- 384
- Langue:
- Anglais
- Collection :
Caractéristiques
- EAN:
- 9780262572262
- Date de parution :
- 16-06-06
- Format:
- Livre broché
- Format numérique:
- Trade paperback (VS)
- Dimensions :
- 159 mm x 228 mm
- Poids :
- 544 g