- Retrait gratuit dans votre magasin Club
- 7.000.000 titres dans notre catalogue
- Payer en toute sécurité
- Toujours un magasin près de chez vous
- Retrait gratuit dans votre magasin Club
- 7.000.000 titres dans notre catalogue
- Payer en toute sécurité
- Toujours un magasin près de chez vous
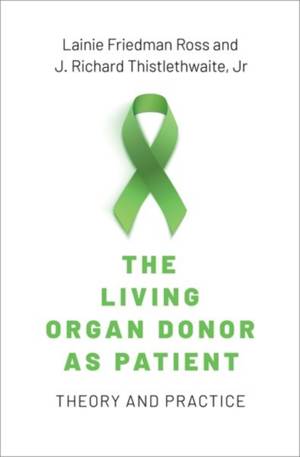
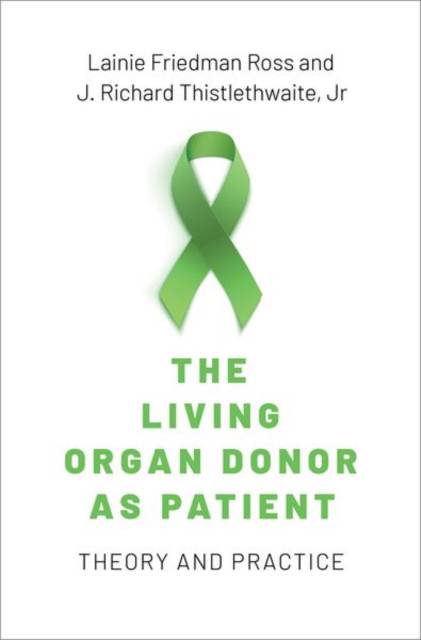
The Living Organ Donor as Patient
Theory and Practice
Lainie Friedman Ross, J Richard Thistlethwaite Jr
Livre relié | Anglais
98,45 €
+ 196 points
Description
When Joseph Murray performed the first successful living kidney donor transplant in 1954, he thought this would be a temporary stopgap. Today, we are no closer to the goal of adequate organ supply without living donors--if anything, the supply-demand ratio is worse. While most research on the ethics of organ transplantation focuses on how to allocate organs as a scarce medical resource, the ethical treatment of organ donors themselves has been relatively neglected. In The Living Organ Donor as Patient: Theory and Practice, Lainie Friedman Ross and J. Richard Thistlethwaite, Jr. argue that living donor organ transplantation can be ethical provided that we treat living solid organ donors as patients in their own right. Ross and Thistlethwaite develop a five-principle framework to examine some of the attempts to increase living donation. It uses the three principles of the Belmont Report: respect for persons, beneficence, and justice modified to organ transplantation, as well as the principles of vulnerability and special relationships creating special obligations. Their approach requires that the transplant community fully embrace current and prospective living organ donors as patients to whom we have special obligations. Only when living organ donors are regarded as patients in their own right and have a living donor advocate team dedicated to their well-being can the moral limits of living solid organ donation be realized and living donors be given the full respect and care they deserve.
Spécifications
Parties prenantes
- Auteur(s) :
- Editeur:
Contenu
- Nombre de pages :
- 408
- Langue:
- Anglais
Caractéristiques
- EAN:
- 9780197618202
- Date de parution :
- 14-12-21
- Format:
- Livre relié
- Format numérique:
- Genaaid
- Dimensions :
- 165 mm x 246 mm
- Poids :
- 680 g